Living with ulcerative colitis (UC) can be challenging. It’s especially true when it comes to managing your diet. This chronic inflammatory bowel disease affects the colon and rectum, but not the small bowel. Symptoms include abdominal pain, diarrhea (commonly with blood), fatigue, and weight loss.
Certain foods may help reduce inflammation, ease digestion, and promote gut health. So it’s essential to know the best foods for ulcerative colitis.
Ulcerative Colitis and Nutrition
Ulcerative colitis involves flare-ups followed by periods of remissions. During a flare-up, your digestive system becomes highly sensitive. It’s then essential to choose foods that are not harmful to your gut. While, during remission, you may tolerate a wider variety of foods. Nutrition is critical in managing UC. The best foods for ulcerative colitis vary from person to person. Consulting a registered dietitian or healthcare provider is always recommended.
So, what are the best foods for ulcerative colitis?
These are the recommended foods for ulcerative colitis patients
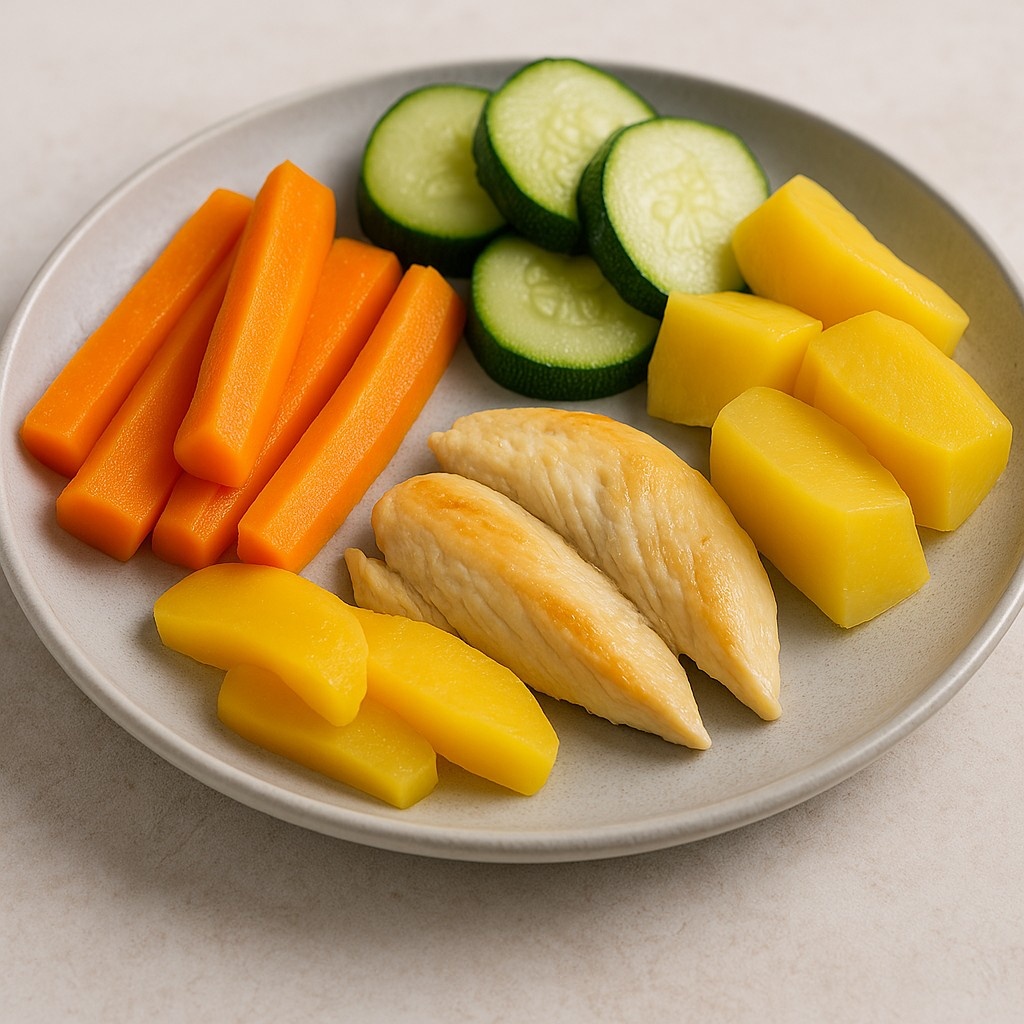
1. Low-Fiber Fruits and Vegetables
Fiber is a healthy nutrient, but during an ulcerative colitis flare-up, it’s better to avoid them. Fiber foods irritate the digestive tract. Low-fiber foods include:
Cooked vegetables: Carrots, zucchini, spinach, and squash.
Soft fruits: Bananas, melons, peaches, and applesauce.
Avocado: Rich in healthy fats and easy to digest.
These foods provide essential vitamins. They provide also minerals, and they cause no adverse effects on your gut.
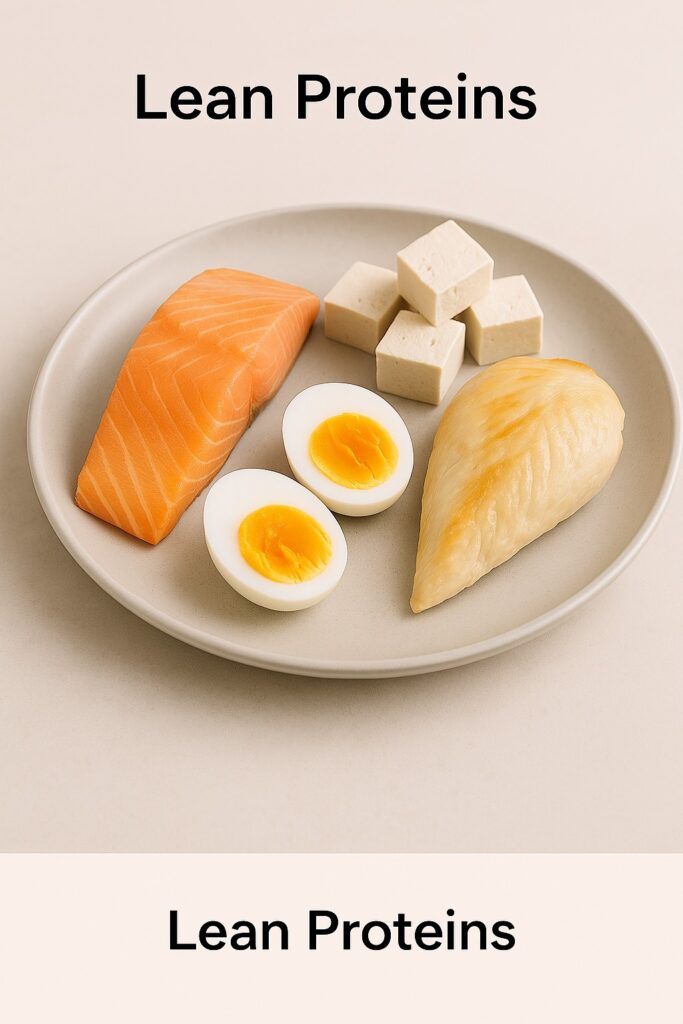
2. Lean Proteins
Lean proteins are undoubtfully one of the best foods for ulcerative colitis. Protein is important for repairing tissues. Maintaining muscle mass also requires protein. This is particularly important if you have weight loss due to UC. Select lean protein sources that are less likely to trigger inflammation. These include:
White meats: Skinless chicken and turkey.
Fish: Salmon, cod, and other fatty fish rich in omega-3 fatty acids. Omega-3 fatty acids have anti-inflammatory properties.
Eggs: Soft-boiled or scrambled eggs are easy to digest.
Plant-based proteins: Tofu and tempeh. These may not be tolerated by some people.
Red meat and processed meat can exacerbate inflammation, so it should be better avoided.
3.Refined Grains
While whole grains are generally healthier, they can be hard to digest especially during a UC flare-up. Instead, you can consume refined grains which are easier to digest:
Refined grains are the following:
– White rice
– Oatmeal (plain, not instant)
– Gluten-free bread (if gluten sensitivity is present)
Once your symptoms improve, you can gradually reintroduce small amounts of whole grains like quinoa or brown rice.
4. Healthy Fats
Fats are an excellent source of energy. However, greasy or fried foods can worsen symptoms of ulcerative colitis. The following are sources for healthy fats, and they help in the absorption of fat-soluble vitamins like A, D, E, and K:
– Olive oil
– Coconut oil
– Nuts and seeds (in moderation and only during remission)
– Avocado
5.Probiotic-Rich Foods
Probiotics help restore the balance of good bacteria in your gut. This will reduce inflammation and improve digestion.
Probiotic-rich foods include yogurt (with low in added sugars), kefir, sauerkraut, Miso soup, kimchi (if tolerated)
6.Hydration
Dehydration is a common concern for patients with UC. During flare-ups dehydration results from diarrhea. Drink plenty of fluids throughout the day to keep well hydrated.
Good drinks (in addition to at least 8–10 glasses of water daily) include:
Herbal teas: Chamomile and peppermint tea.
Electrolyte (salts) drinks: Coconut water or oral rehydration solutions are helpful to replace lost electrolytes.
Avoid caffeine, alcohol, and sugary beverages, as they cause gut irritation.

Avoid the following foods during flare-ups of your disease:
– Spicy foods
– Dairy products (if lactose intolerant)
– High-fiber foods (raw vegetables and nuts, as examples)
– Carbonated drinks
– Processed snacks (high in sugar and unhealthy fats)
The Role of Supplements
Patients with UC may have nutrient deficiencies. Supplements may then be necessary, including iron, vitamin D, calcium, and omega-3fatty acids.
Conclusion
Managing ulcerative colitis through diet is important. Patients must focus on easily digestible foods and avoid known triggers. Of course, medications are the cornerstone of managements, but a strict dietary plan is also necessary, to improve quality of life and to control symptoms in flare ups of the disease.

