Irritable Bowel Syndrome (IBS) is a chronic disorder. It often disturbs the normal daily life and affects millions worldwide. It’s characterized by a cluster of symptoms including abdominal pain, bloating, gas, and altered bowel habits (constipation, diarrhea, or both). IBS may significantly affect a person’s quality of life. Probiotics in the treatment of irritable bowel syndrome is becoming more and more accepted as a treatment option.
The exact cause remains unknown, but there is growing evidence pointing to a disturbed gut microbiome. Microbiome a term denoting the microorganisms living in our intestines, which are considered as a key player as a possible cause of IBS. Probiotics (live microorganisms with proven health benefits) are said to be a promising treatment option.
What’s the Gut-Brain Axis? And How Is It Connected To Irritable Bowel Syndrome?
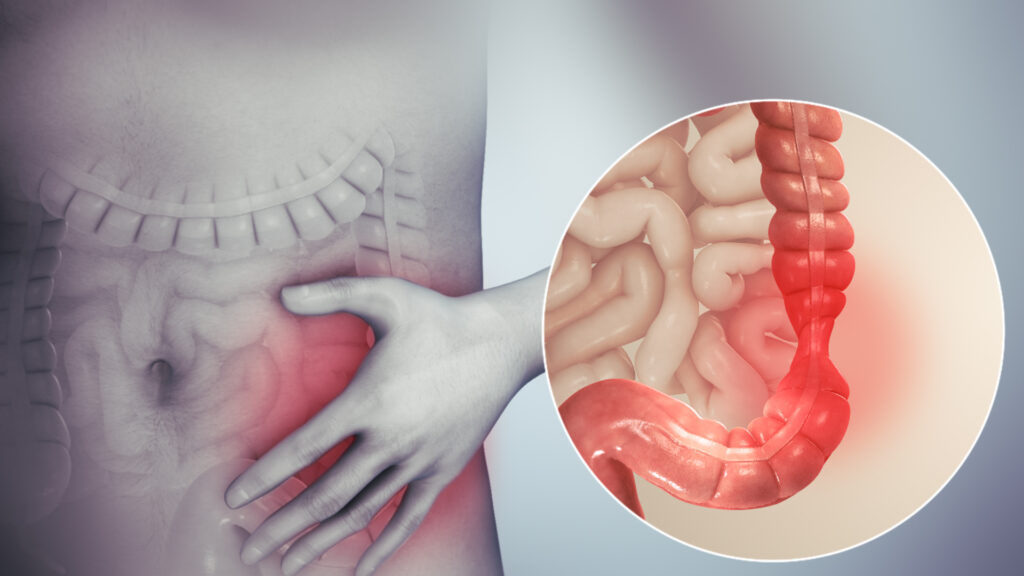
The gut and brain are linked together through a complex communication of neural network known as the gut-brain axis. In individuals with IBS, this communication may function in an abnormal way. When this happens, it may lead to visceral hypersensitivity (increased pain perception in the gut). It may also result in dysregulation (disturbance of the normal control) of gut motility.
Furthermore, the gut microbiota plays a central role in producing substances known as neurotransmitters (chemicals that are involved in nerve impulses transmission). Microbiota also regulate immune responses and maintain the integrity of the bowel lining (so that harmful substances present in the gut lumen can’t enter the gut wall and cause troubles).
When the balance of “good” and “bad” bacteria is disrupted (this is called dysbiosis) – it can make IBS symptoms worse. Many persons who suffer from IBS have less numbers of some beneficial) bacteria. (like Lactobacillus and Bifidobacterium species).
How Do Probiotics Cause Relief of Symptoms of Irritable Bowel Syndrome?
Probiotics work through different mechanisms to relieve IBS symptoms:
- Restoring Microbial Balance: When you consume probiotics, you introduce beneficial bacteria to your gut. Subsequently, the healthy microbial balance will be restored, and the harmful (bad) bacteria will no longer cause disturbing symptoms.
- Strengthening the Gut Barrier: The bowel or gut lining functions as a protective barrier. It prevents harmful substances from entering the bloodstream. Probiotics can result in more production of mucus and strengthening of the tight junctions between intestinal cells. When these junctions are strong the gut becomes no more “leaky”, and harmful substances can’t enter the bloodstream.
- Adjusting the Immune System: Many people with IBS have some degree of mild inflammation in the gut. Probiotics can alter and adjust the immune response, so that inflammation is suppressed, and symptoms are reduced.
- Producing Beneficial Substances: Probiotics act on dietary fiber and produce Beneficial fats called short-chain fatty acids (a process known as fermentation). An example of these fatty acids is butyrate. Short-chain fatty acids are good energy source for colon cells. In addition, they have anti-inflammatory properties (i.e. suppress inflammation). Some probiotic strains can also produce antimicrobial substances. They substances kill harmful bacteria.
- Decreasing Visceral Hypersensitivity (pain perception in the gut): Some probiotics directly act on the nerves in the gut and reduce the abnormally high level of pain sensation experienced by IBS patients.
Which Probiotic Strains are best for Irritable Bowel Syndrome patients?
Not all probiotics are the same. They vary in effectiveness according to the strain of “good” bacteria that the probiotic consist of. Some strains are more beneficial for IBS.
These are the most promising strains:
- Bifidobacterium infantis 35624: Very effective to reduce IBS symptoms, including abdominal pain and bloating.
- Lactobacillus plantarum 299v: Useful in treating abdominal pain, bloating, and flatulence. It can improve gut motility, therefore helpful for IBS with constipation.
- Saccharomyces boulardii: A yeast probiotic (not bacteria). It’s effective for IBS with diarrhea and for IBS which is caused by infectious diarrhea (some IBS patients develop their symptoms after acute gastroenteritis. This probiotic reduce abdominal pain and frequency of bowel motions.
- Lactobacillus acidophilus NCFM® and Bifidobacterium lactis Bi-07®: These strains are usually found in combination. They regulate bowel motions and reduce bloating and cramps.
- Bacillus coagulans: Different strains of this species may be of good benefit for relief of symptoms like abdominal pain, and bloating.

What Important Considerations Should We consider?
In general, probiotics in the treatment of irritable bowel syndrome should be taken regularly for at least 3-4 weeks to assess their effectiveness. If symptoms get worse or new symptoms appear, it’s best to discontinue using probiotics, and to seek medical advice.
The research on probiotics for the treatment of IBS continues. There is hope for more effective treatments in the future. The way by which probiotics cause relief in symptoms depends on the type of probiotic strains. When particular strains are found to help improve specific IBS symptoms, treatment can be more targeted, by choosing the right probiotic species for the specific symptoms.


Pingback: The Best Foods for Patients with Crohn’s Disease - GutConsultant
Pingback: Burping and gases: How to treat? - GutConsultant burping, excessive gas